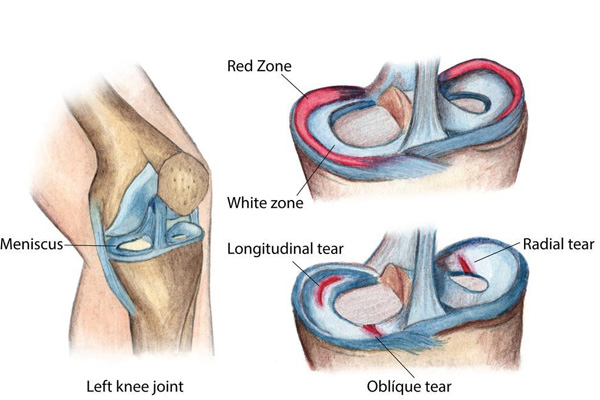
A meniscus root tear is a specific type of tear that occurs at the attachment site of the meniscus to the tibia (shinbone). The meniscus is a C-shaped piece of cartilage in the knee that acts as a cushion between the femur (thighbone) and tibia, helping with shock absorption and load distribution. The "roots" of the meniscus are where it is anchored to the bone.
Types of Meniscus Root Tears:
- Posterior Root Tears: These are the most common and occur at the back attachment of the meniscus.
- Anterior Root Tears: These occur at the front attachment, but they are less common.
Mechanism of Injury:
Meniscus root tears can happen due to several factors:
- Traumatic Injury: A sudden, forceful twist or pivot of the knee, often seen in athletes participating in sports like soccer, basketball, or skiing.
- Degeneration: In older adults, meniscus root tears can occur due to wear and tear over time, where the meniscal tissue becomes weaker.
Symptoms:
- Pain: Deep, sharp pain in the knee, especially with activities like squatting, going up or down stairs, or deep knee flexion.
- Swelling: The knee may become swollen after the injury.
- Mechanical Symptoms: Some patients may experience "locking" or "catching" in the knee, where it feels like the knee gets stuck.
- Instability: The knee may feel less stable when walking or performing weight-bearing activities.
Importance of the Meniscus Root:
The root of the meniscus is crucial because it anchors the meniscus and allows it to perform its function of distributing load and absorbing shock. When the root is torn, the meniscus can become displaced, rendering it ineffective. This is often referred to as a "functional meniscectomy," meaning the meniscus is no longer able to protect the knee joint, leading to:
- Increased stress on the cartilage.
- Accelerated osteoarthritis development.
- Loss of knee stability.
Diagnosis:
- MRI: An MRI scan is the primary imaging tool to confirm a meniscus root tear, as it provides detailed images of the soft tissues in the knee.
- Physical Exam: Clinicians may also use specific clinical tests to assess the meniscus, though root tears are not always easily detected through physical examination alone.
Treatment:
- Non-Surgical Treatment: In some cases, especially in older patients with degenerative tears, conservative management might be considered. This can include physical therapy, anti-inflammatory medications, and activity modification.
- Surgical Treatment: For younger, active individuals or those with traumatic meniscus root tears, surgery is often recommended. Surgical options include:
- Meniscus Root Repair: This involves suturing the torn root back to its original attachment site on the tibia.
- Partial Meniscectomy: In some cases, part of the damaged meniscus may be removed if it cannot be repaired.
Meniscus root tears are significant because, without proper treatment, they can lead to early osteoarthritis and loss of knee function, particularly in active individuals.






